An autoclave is a powerful and useful device in a variety of fields, particularly in the medical, scientific, and industrial sectors. But how does an autoclave work? Well, its primary function is to sterilise equipment and supplies, ensuring that they are free from microorganisms that could potentially cause harm or interfere with results in a laboratory setting.
The process of sterilisation in an autoclave is achieved by subjecting its contents to high-pressure saturated steam. This steam is typically at temperatures of about °C or more, a heat level that is lethal to bacteria, viruses, fungi, and spores.
The exposure to this steam happens over a period of time, typically for about 15-20 minutes. However, the exact duration can vary depending on the load size and the contents undergoing sterilisation.
The autoclave’s ability to reach such high temperatures under pressure sets it apart from other sterilising methods, such as boiling or using dry heat, which may not be as effective at eliminating resilient microorganisms.
A Deep Dive Into How An Autoclave Works
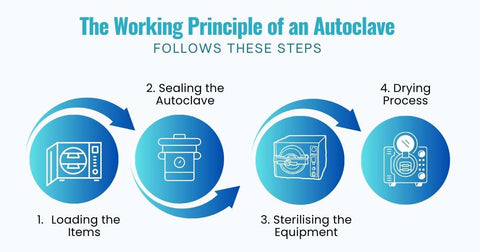
The working principle of an autoclave is relatively straightforward:
Loading The Lab Items
The process begins with the loading of the items to be sterilised. First, individuals thoroughly clean these items to remove any present debris or dirt. This is a crucial step because any residual material could potentially shield microorganisms from the sterilising effects of the autoclave.
Once cleaned, the individuals carefully arrange the items inside the autoclave chamber. The arrangement is done in such a way that allows for the free circulation of steam, ensuring that all surfaces of the items come into contact with the steam.
Sealing The Autoclave and Heating
After loading, the operators seal the autoclave to create a closed system. This is important to prevent the escape of steam during the sterilisation process. The autoclave is then heated, which causes the water inside to vaporise, creating steam. The generation of steam is a critical aspect of the autoclave’s operation, as it is the steam that carries out the sterilisation.
Sterilising The Apparatus
The generated steam is then pressurised and distributed evenly throughout the chamber. The combination of heat, steam, and pressure is lethal to a wide range of microorganisms, including bacteria, viruses, and spores.
The high temperature of the steam denatures the proteins in these microorganisms, effectively killing them. The pressurised nature of the steam ensures that it penetrates all areas of the items, including crevices and interior spaces, ensuring thorough sterilisation.
Drying
After completing the sterilisation process, which typically lasts for about 15-20 minutes but can vary depending on the size of the load and the type of items, the chamber vents out the steam. This depressurises the autoclave and allows the items inside to dry. Drying is an important final step in the process, as it prevents the growth of microorganisms that might occur in a moist environment.
What Makes Autoclaving Better Than Boiling?
Before the invention of an autoclave, the preferred sterilisation methods were boiling, dry heat or open flame, and the use of sterilisation chemicals. One of the oldest and simplest methods of sterilisation was boiling. People boiled items in water for a certain period of time to kill microorganisms.
However, boiling is ineffective against all types of microorganisms, especially certain spores and viruses.
Some were heating lab equipment in an oven or over an open flame. While this method can be effective, it requires longer exposure and higher temperatures than moist heat sterilisation. One of the risks with this method too, was the danger of open flames.
Lastly, chemicals such as hydrogen peroxide, nitrogen dioxide, and formaldehyde sterilised lab items. These chemicals can kill a wide range of microorganisms, but they can be a health hazard and may leave residues.
So, when Dr. Charles Chamberland invented the autoclave in 1879, autoclaving became preferred over boiling for sterilisation due to several key advantages:
Steam Is More Efficient
Autoclaving is more effective at killing microbes and more efficient in terms of time because of steam. Unlike boiling, which may require a very long period of time or intermittent boiling to kill certain microorganisms, autoclaving can achieve sterilisation in a shorter time frame.
Steam is highly effective at eliminating microorganisms. The reason behind this is when steam comes into contact with an object that is cooler, it changes back into water. During this condensation process, the cooler object directly receives all the energy that initially converted the water into steam.
This energy transfer heats up the cells of the microorganisms much more efficiently than air would at the same temperature. This superior heat transfer efficiency is why steam is the preferred medium for achieving sterility.
Higher Temperatures
Autoclaves can reach temperatures of around 121°C to 135°C, which is significantly higher than the boiling point of water at 100°C. This higher temperature allows autoclaves to kill a wider range of microorganisms, bacteria, and pathogens, including those that are resistant to the temperature of boiling water.
Pressurisation Kills Microorganisms
Autoclaves use pressurised steam in addition to high temperatures to sterilise items. This method can penetrate deeper into materials, ensuring a more thorough sterilisation process. In contrast, boiling can only sterilise the outer parts of the lab equipment.
Kills Resistant Microorganisms
Autoclaving can kill spores and germs that are normally resistant to boiling water and even powerful detergents. Boiling can kill almost everything except some endospores.
Suitable For All Shapes & Sizes
The steam used in autoclaving can reach all the nooks and crannies of all kinds of instruments, making it suitable for sterilising items of various shapes and sizes.
Environmental Friendliness & Less Health Risk
Autoclaving only uses water and heat to kill off foreign materials, so there is no risk of harmful emissions. Plus, the lack of chemical usage means that lab personnel won’t have to worry about getting in contact with various cleaning chemicals.
What Lab Equipment Are Autoclavable?
An autoclave can sterilise a wide range of laboratory equipment. Here are some examples:
- Glassware: This includes beakers, flasks, test tubes, petri dishes, and other glass instruments.
- Metal Instruments: Tools made of metal, such as scissors, forceps, scalpels, and spatulas, can be autoclaved.
-
Surgical and Dental Instruments: These are often made of stainless steel and can withstand the high temperatures of an autoclave.
-
Laboratory Clothing: Lab coats and gloves can be autoclaved to ensure they are free of any potential contaminants.
-
Biohazard Waste: Autoclaves are often used to sterilise biohazardous waste before it is disposed of.
-
Culture Media and Reagents: These are often autoclaved to ensure they are sterile before use.
-
Pipettes and Pipette Tips: Pipettes and tips can be autoclaved to ensure they don’t contaminate samples.
- Plasticware: Certain plasticware that can withstand high temperatures can also be autoclaved. Some plastics, for example, may melt or warp. Always check the manufacturer’s instructions before autoclaving any item.
-
Biological Safety Cabinets: These are often decontaminated using an autoclave before being repaired or moved.
It’s important to note that not all materials can withstand the high temperatures and pressure of an autoclave. If unsure, don’t hesitate to contact your manufacturer or laboratory equipment supplier like us, Science Equip.
By choosing Science Equip, we guarantee that our lab apparatus is of the highest safety and durability standards. If you want to verify whether the plasticware or any lab item you bought from us is autoclavable, just send us a message here.